Post-sale Broker Services
Streamline prospecting and submitting new clients with Paragon’s group sales and renewal services.
Why partner with paragon
Lorem ipsum dolor sit amet consectetur. Viverra dolor eget posuere mauris viverra.
Lorem ipsum dolor sit amet consectetur. Tellus a molestie nunc dictum nulla. Vulputate interdum pretium adipiscing pellentesque. Amet facilisi quam a malesuada adipiscing.
Comprehensive Benefit Administration Management
Eligibility & Billing
Eligibility maintenance, enrollment audits, and carrier billing are reconciled across carriers and ben-admin platforms, maintaining ongoing accuracy post-sale.
Claims Advocacy
Complex or escalated claims are engaged directly with carriers, leveraging established relationships and escalation pathways to support timely review and resolution when standard channels stall.
Renewals
Carrier renewals are managed end-to-end, beginning with renewal delivery and review, incorporating claims experience analysis and market pricing validation, evaluating plan design and cost-mitigation options, and carrying changes through open enrollment and final carrier processing.
Ben-Admin
Benefit administration systems are actively managed across platforms like Employee Navigator, including wall notices, plan ID updates, carrier integrations, and discrepancy reports—maintaining system integrity post-sale.
Compliance
Post-sale compliance is delivered through Paragon’s HR partner ecosystem, combining small-group compliance tools and documentation with education and consultation on ACA reporting for level-funded and large employer groups—built for scale and evolving regulatory requirements.
Ongoing Broker Support
Day-to-day broker support is provided for plan questions, ID card requests, carrier inquiries, documentation needs, and service continuity—serving as a consistent point of contact post-sale.
Lorem Ipsum Dolor
Locations Lorem Ipsum Dolor
Lorem ipsum dolor sit amet consectetur. In vitae arcu semper eros blandit aliquet. Lacus et orci convallis in mollis.
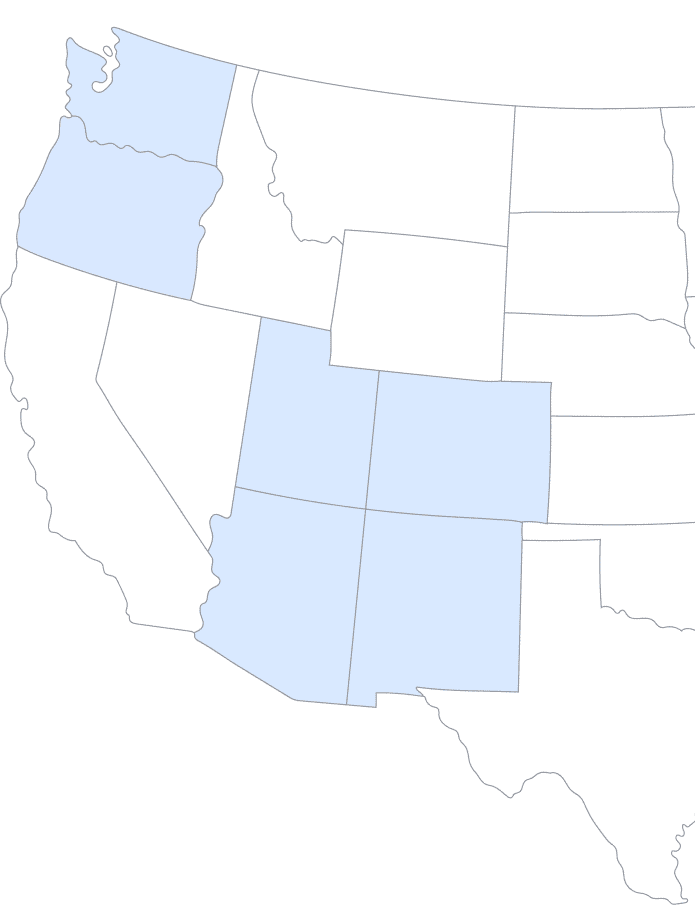

Lorem ipsum dolor sit amet consectetur. Non at pellentesque dui fermentum mauris id justo lorem augue. A tortor vitae amet mattis risus blandit. Diam odio sapien eget vivamus. Ut aliquam odio praesent vitae laoreet. Pulvinar proin tellus adipiscing sagittis.
Jared Jones, Company Name
product offerings
Lorem ipsum dolor sit amet consectetur.
Frequently asked questions
Yes. Paragon remains actively engaged post-sale, managing eligibility, billing accuracy, benefit administration, renewals, claims advocacy, and day-to-day service support—ensuring continuity and operational stability throughout the life of the group.